At the Neuroendocrine and Carcinoid Tumors Program at Dana-Farber Brigham Cancer Center, our goal is to improve the lives of people with neuroendocrine tumors by offering patients a comprehensive range of services based on specialized treatments and innovative research. Our novel therapies and clinical trials give our patients access to the latest and most sophisticated therapies tailored to their tumor.
In the Neuroendocrine and Carcinoid Tumors Program, our experts specialize in the treatment of neuroendocrine tumors, while continually developing new and better therapies for the future.
Our program's highly specialized clinical team is made up of experts from two world-class medical centers — Dana-Farber Cancer Institute and Brigham and Women's Hospital — who are changing the way neuroendocrine tumors are studied, diagnosed, and treated. Because we are such a specialized center, we focus on the distinct needs of people with neuroendocrine tumors. This enables us to provide a very personalized approach to care for our patients.

Our specialists work closely together to offer coordinated, advanced treatments, including access to novel therapies that were discovered in our own labs, and several clinical trials.
We offer an approach to treatment that includes:
- A team of oncologists specializing in neuroendocrine tumors.
- A multidisciplinary approach to care based on each patient's unique situation.
- Highly advanced diagnostic procedures.
- Complex surgical procedures.
- Interventional radiology techniques, including embolization.
- Access to leading-edge clinical trials.
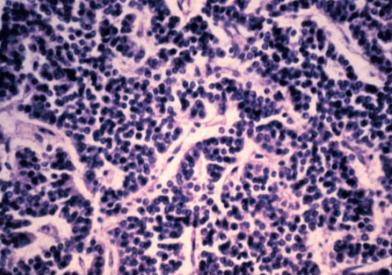
- Pathologic and molecular testing of tumor specimens.
- Genetic testing and counseling for families with a cancer history.
- Easy access and timely appointments.
Innovative Approach
Investigators in the Neuroendocrine and Carcinoid Tumors Program have a proven track record of discovering new and promising treatment options. Our physician-scientists' research informs our approach to your individual treatment. We use Dana-Farber Cancer Institute's neuroendocrine tumor database — the largest of its kind — to study the molecular mechanisms underlying the growth and development of neuroendocrine tumors. We are using this database to develop neuroendocrine tumor cell lines, with the goal of using these models to test new biologic hypotheses and evaluate new drugs.
Our innovative approach is also reflected in our collaborative, multi-disciplinary model of care that includes some of the best practitioners in every medical discipline. Specialists from gastroenterology, pathology, radiology, surgical oncology, surgery, medical oncology, radiation oncology, nursing, research and other specialties meet regularly to review all approaches to treatment, and to ensure that patients receive the best care plan and most effective treatment.
The program's experts are leaders in their fields, regularly publishing their discoveries about new therapies, underlying mechanisms of these diseases, genetic discoveries, risk factors, and early detection.
Compassionate Care
At Dana-Farber Brigham Cancer Center, we view every patient as an individual, with unique needs and expectations. This understanding guides us in creating a treatment plan that takes your lifestyle and goals into account. Our team is committed to finding the very best way to help patients and their families cope with the physical and emotional effects of neuroendocrine tumors and their treatment.
Our patients have access to a wide range of services, including nutrition counseling, rehabilitation, and physical therapy. We also understand that cancer affects more than the body. We offer many support programs and resources that help patients and families, including integrative therapies such as massage and acupuncture.