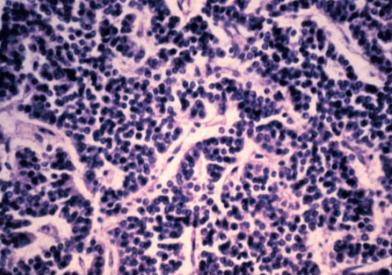
Neuroendocrine tumors (NETs) develop from specialized, hormone-producing neuroendocrine tissue distributed throughout the body. They can form in the gastrointestinal tract, lungs, pancreas, and other tissues.
- NETs are also known as carcinoid tumors, especially when they grow out of the gastrointestinal tract or lungs.
- Pancreatic NETs are sometimes called "islet cell" tumors and include insulinomas, glucagonomas, gastrinomas, VIPomas, and non-functioning NETs.
- Some NETs secrete hormones, while others do not. Those secreting hormones are referred to as functioning and may cause specific symptoms related to that hormone's excessive production.
- Most NETs grow slowly, but some are more aggressive, grow rapidly, and spread to other parts of the body.
At Dana-Farber/Boston Children's Cancer and Blood Disorders Center, our pediatric cancer specialists have the experience and expertise to treat neuroendocrine tumors in our Endocrine-Oncology Program. Our multidisciplinary team will provide your child with the best possible care from diagnosis through treatment and beyond.
Causes and Symptoms of Childhood Neuroendocrine Tumors
Some neuroendocrine tumors result from hereditary factors. Examples of hereditary or genetic conditions that carry an increased risk for developing NETs include:
- Multiple endocrine neoplasia (MEN)
- Familial medullary thyroid cancer (FMTC) syndrome
- von Hippel-Lindau syndrome
- Hereditary pheochromocytoma and paraganglioma syndromes
- Carney triad
Symptoms caused by a neuroendocrine tumor may vary from child to child. They will depend on the tumor's location, size, and type, including the type of hormone it secretes. Symptoms might mimic other, more common ailments.
Some of the most common symptoms include:
- Abdominal pain that resembles appendicitis if the tumor is in the appendix.
- High blood pressure, dizziness, heart palpitations, nausea, vomiting, or excessive sweating if the tumor is pheochromocytoma or paraganglioma.
- Abdominal pain, stomach ulcers, vomiting, diarrhea, and weight changes for NETs of the pancreas or GI tract.
- A lump or swelling in the neck, difficulty breathing or swallowing, or hoarseness of the voice if the tumor is medullary thyroid cancer.
- Pain or feeling full near the site of the tumor if the tumor is large.
If your child has any of these symptoms, call your doctor for an evaluation right away.
How We Diagnose Childhood Neuroendocrine Tumors
The first step of an effective treatment plan is an accurate diagnosis. We order as many diagnostic tests as necessary to confirm a diagnosis. These tests may include imaging studies, biopsy, and blood and urine tests.
If your child needs any additional testing, your doctor will discuss their recommendations with you. Once we have an accurate and complete diagnosis, we will develop a treatment plan that meets your child's unique needs.
How We Treat Childhood Neuroendocrine Tumors
We take an integrated approach to treating neuroendocrine tumors. Your child will see specialists across oncology, endocrinology, radiation therapy, and surgery, who will work together throughout your child's treatment.
Neuroendocrine tumors treatment may include:
- Surgery: We perform surgical procedures to biopsy the tumor and remove the tumor and nearby tissue.
- Radiation therapy: We use radiation therapy before or after surgery to damage or eliminate cancer cells and shrink tumors. Your child's condition will determine whether radiation therapy is necessary.
-
Chemotherapy: We may also use chemotherapy as a treatment to destroy or shrink cancer cells. Similar to radiation therapy, we may use it before or after surgery.
Different groups of chemotherapy drugs work in different ways. Often, we will use a combination of chemotherapy drugs. Your child may receive chemotherapy:
- Orally, as a pill to swallow.
- Intramuscularly, as an injection into the muscle or fat tissue.
- Intravenously, as a direct injection into the bloodstream or IV.
- Intrathecally, as a direct injection into the spinal column through a needle.
While chemotherapy can be very effective in treating certain cancers, the treatment can't differentiate normal healthy cells from cancer cells. As a result, there can be adverse side effects during treatment. Being able to anticipate these side effects can help the care team, child, and family prepare for, and in some cases prevent these complications from occurring.
- Genetic counseling: We help your child and family cope with the stress of a hereditary cancer diagnosis while discussing practical considerations such as future reproductive options.
As your child transitions from treatment to life after treatment, we continue to care for them in our pediatric cancer survivorship programs. We conduct regular medical evaluations and provide patient and family education, support groups, and a wide variety of counseling services.