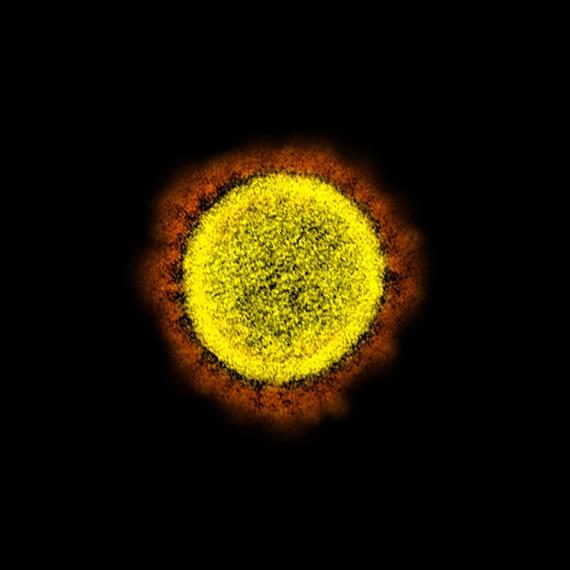
Multinational study identifies high risk to cancer patients diagnosed with COVID-19
- Largest series to date looks at nearly 1000 cancer patients also diagnosed with COVID-19
- Study identifies risk factors unique to cancer patients
People with cancer sickened by COVID-19 have a crude death rate of 13%, according to the largest series of data released thus far from a multinational perspective. The data on more than 900 patients, published in The Lancet, also revealed cancer-specific factors associated with increased mortality.
The information is the first report from an ongoing international initiative by the COVID-19 and Cancer Consortium (CCC19) to track outcomes within this vulnerable population. Dana-Farber Cancer Institute is one of five founding institutions of CCC19.
“The report tracks patients from a broad geographic distribution and across practice settings,” said Dana-Farber’s Toni K. Choueiri, co-lead author of the study and CCC19 steering committee member. Choueiri is the director of the Lank Center for Genitourinary Oncology and the Jerome and Nancy Kohlberg Professor of Medicine at Harvard Medical School.
“We find significant associations with increased 30-day all-cause mortality in addition to previously reported factors such as age and gender,” said Choueiri. “This has implications for patients and healthcare providers that deal with cancer patients.”
The death rate for this group of patients as a whole was 13%, more than twice that reported for all patients with COVID-19 (by the Johns Hopkins Center for Systems Science and Engineering), the study authors said. Certain subgroups, such as patients with active (measurable) cancer and those with an impaired performance status, fared “much, much worse.”
The data in this first report from CCC19 was gathered from 928 patients in Spain, Canada and the majority from the United States.
The cancer-specific factors associated with increased mortality included having an ECOG performance status of two or worse. ECOG is a grading scale for measuring how cancer impacts a patient’s daily living abilities. A score of two designates a patient who is capable of selfcare but unable to work and who is up and about more than 50% during waking hours. Another factor associated with increased mortality was an active cancer status, particularly progressive cancer. The mortality risk also increased with the number of comorbidities, such as hypertension or diabetes, particularly with two or more comorbidities. As is the case with the non-cancer population, mortality increased with age. Mortality was 6% for cancer patients younger than 65, 11% for those 65-74 and 25% for those older than 75. Males also had a higher death rate than females, 17% compared to 9%.
These early data showed no statistical association between 30-day mortality and cancer treatments, suggesting that surgery, adjuvant chemotherapy and maintenance chemotherapy could continue during the pandemic with “extreme caution.” “While older patients and those with major comorbid conditions are at substantially increased risk of dying from COVID-19, our early findings are encouraging news for patients without major medical conditions who receive their cancer therapy within four weeks of their infection. However, more data are needed to reliably assess individual higher risk therapies,” the researchers said.
The study’s corresponding author is Jeremy Warner, MD, MS, associate professor of Medicine and Biomedical Informatics at Vanderbilt University. Other lead authors are Brian Rini, MD, Ingram Professor of Cancer Research and Chief of Clinical Trials at Vanderbilt-Ingram Cancer Center; Gary H. Lyman, MD, MPH, professor of Medicine-Oncology at the University of Washington; Nicole Kuderer, MD, with the Advanced Cancer Research Group in Seattle; Dimpy Shah, PhD, MBBS, MSPH, assistant professor of Epidemiology and Biostatistics at Mays Cancer Center, home to UT Health San Antonio MD Anderson; and Yu Shyr, PhD, the Harold L. Moses Chair in Cancer Research and chair of the Department of Biostatistics at Vanderbilt.
CCC19 was formed to rapidly collect data as part of an effort to understand the unique effects the coronavirus has on people with cancer. Participants include members of the European Society of Medical Oncology (ESMO), institutions that are National Cancer Institute Designated Cancer Centers, researchers from several nations as well as community-based oncologists within the United States. More than 100 institutions have signed up in the United States and Canada. ESMO is coordinating efforts in Europe through ESMO-CoCare registry.
Media Contacts
If you are a journalist and have a question about this story, please call 617-632-4090 and ask to speak to a member of the media team, or email media@dfci.harvard.edu.
The Media Team cannot respond to patient inquiries. For more information, please see Contact Us.