Incidence
- The incidence of melanoma is increasing worldwide.
- Melanoma is most common in adults, but it is sometimes found in children and adolescents. About 300 children in the United States are diagnosed with melanoma each year.
- Although skin cancer is the most common cancer in the United States, melanoma accounts for less than 2 percent of all skin cancer cases. Basal cell carcinoma and squamous cell carcinoma are more common skin cancers than melanoma.
- Although the least common type of skin cancer, melanoma is more likely to spread (metastasize) to other parts of the body.
Growth and Spread
If melanoma grows at the site of the original tumor, it tends to grow in one of two ways:
- Radial growth: The melanoma spreads horizontally along the top layers of your skin. Most melanomas start growing this way, but some may eventually grow into deeper layers of your skin.
- Vertical growth: The melanoma grows into deeper layers of skin. This kind of growth is more serious and may spread to other parts of the body. Nodular melanoma grows this way fairly quickly, but most other types grow along the top layers of skin first for some time.
Risk Factors
Anything that increases your risk of getting a disease is called a risk factor. Having a risk factor does not mean that you will get cancer; not having risk factors doesn't mean that you will not get cancer. Talk with your doctor if you think you may be at risk for melanoma.
The biggest risk factors for melanoma are:
- Exposure to natural or artificial sunlight (such as tanning beds) over long periods of time
- Fair skin that freckles and burns easily, does not tan, or tans poorly
- Having unusual moles
Other risk factors for melanoma include:
- Family history or a personal history of melanoma
- Ultraviolet radiation (especially from tanning booths)
- Frequent sunburns (especially blistering sunburns)
- Number of moles (more than 50)
- Atypical nevi (unusual moles)
- Immunosuppression
- Blue or green or other light-colored eyes
- Red or blond hair
Symptoms and Signs
Melanoma can vary greatly in appearance. The most important clue in detecting melanoma is a lesion (abnormal lump, bump, ulcer, sore, or colored area on the skin) that is changing and is unlike any other lesion on your skin.
Melanoma often starts with a change in the shape, color, size, or texture of an existing mole or a change in how a pigmented area looks. It may also appear as a new mole. Although melanoma is typically a brown/black color, less commonly, it may appear as a pink, fast-growing, shiny bump.
Photographs used by permission: National Cancer Institute
These and other signs and symptoms may be caused by melanoma or by other conditions. Check with your doctor if you have a mole that:
- Changes in size, shape, or color
- Has irregular edges or borders
- Is more than one color
- Is asymmetrical (if the mole is divided in half, the two halves are different in size or shape)
- Itches
- Oozes, bleeds, or is ulcerated (a hole forms in the skin when the top layer of cells breaks down and the tissue shows through)
Experts recommend using the "ABCDE rule" to help determine when a physician should see a mole or skin change:
- A for asymmetry: One half is differently shaped than the other
- B for border irregularity: Jagged or blurred edges
- C for color: The pigmentation is not consistent
- D for diameter: Moles greater than six millimeters (the size of a pencil eraser)
- E for evolving: A mole changing in size, shape, or color
Screening and Prevention
The Center for Melanoma Oncology at Dana-Farber Brigham Cancer Center aims to raise awareness, provide risk assessment, and promote healthful behaviors. Dana-Farber's Sun Safety/Skin Cancer Prevention Program regularly visits local beaches and outdoor recreation areas in the summer to conduct skin cancer screenings and sun safety education programs. And Dana-Farber's Center for Cancer Genetics and Prevention offers genetic counseling services to determine an individual's risk of developing melanoma or having a hereditary form of the disease.
Screening Recommendations
Ages 18+: You should conduct monthly self-exams to look for new moles and birthmarks, or changes in existing ones. Your physician should evaluate them during your annual exam. If you have a large number of moles, atypical moles, or a family history of melanoma, you should have an evaluation by a dermatologist.
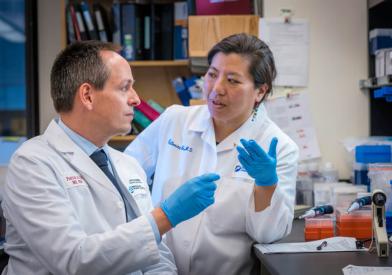
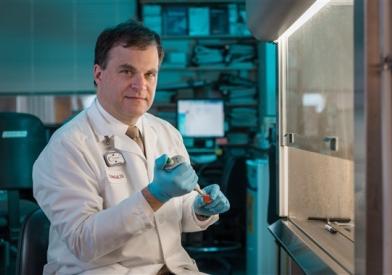
The specialized Center for Melanoma Oncology at Dana-Farber Brigham Cancer Center is a multidisciplinary clinical care center and research hub. Uniting experts in laboratory and clinical research, our center takes a comprehensive approach to conquering this aggressive form of skin cancer.
Our team of experts work together to provide compassionate, comprehensive, and highly coordinated care for patients with melanoma. We offer an extensive array of treatment options, including advanced surgical procedures, radiation therapies, chemotherapy, melanoma clinical trials, immunotherapy, targeted therapies, and the full range of support services from a top-ranked hospital and leading cancer research center.
Our specialists treat the complete spectrum of melanoma subtypes, including rare forms, such as:
- Mucosal melanoma
- Ocular melanoma
- Acral lentiginous melanoma
Other forms we treat include:
- Superficial spreading melanoma
- Nodular melanoma
- Lentigo maligna melanoma
- Desmoplastic melanoma (also known as neurotropic)
- Melanoma of unknown primary
- Atypical spitz/spitzoid melanoma
- Amelanotic melanoma
We provide comprehensive services to patients with these cancers, including:
- Pioneering research in resistance mechanisms, genomic sequencing, and novel immunotherapy approaches
- Clinical trials, including cutting-edge immunotherapy, novel vaccines, targeted therapies, and innovative combinations of therapies, to treat stage III and stage IV melanoma
- Novel interventional techniques, including minimally invasive surgical approaches
- Physician-scientists as part of your team, who work in our labs to develop the best treatments
- Multidisciplinary care delivered by specialists from Dana-Farber Cancer Institute and Brigham and Women’s Hospital