At the Center for Cutaneous Oncology, we believe that each case of skin cancer is as unique as the individual facing the diagnosis. Experts from a wide variety of medical fields are here to evaluate and treat your particular skin cancer, no matter how rare or complex.
As a patient, you are at the center of a dedicated team that works closely together. You'll have access to some of the world's leading skin cancer specialists, including dermatologic oncologists, dermatopathologists, medical oncologists, surgical oncologists, radiation oncologists, radiologists, and other specialists. Together, your team will develop an individualized treatment plan tailored to the stage and particular features of your disease, any general health concerns, and lifestyle considerations.
The experts at the Center for Cutaneous Oncology are dedicated to cancer research, from clinical investigation to basic science, exploring and understanding the fundamental causes of skin cancers.
Diseases Treated
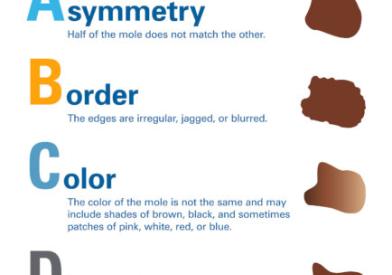
Skin cancers are more common than all other cancers combined, and, collectively, their incidence is rising faster than that of any other cancer. Our Cutaneous Lymphoma, Cutaneous Carcinoma, and Oncologic Dermatology Programs provide highly specialized care for all types of non-melanoma skin cancer, including:
- Cutaneous T cell and B cell lymphoma (CTCL, CBCL)
- Merkel cell carcinoma (MCC)
- Basal cell carcinoma (BCC)
- Squamous cell carcinoma (SCC)
- Rare adnexal neoplasms: eccrine, apocrine, sebaceous, and hair follicle tumors
- Other rare cutaneous cancers
We also treat cutaneous complications of therapy for cancers in general, including:
- Graft-versus-host disease (GVHD)
- Skin reactions to cancer chemotherapy
Immunosuppression and Skin Cancer (ISC) Clinic
Immunosuppressed patients have an elevated risk of skin cancer, a factor particularly relevant for light-skinned patients who have experienced multiple sunburns in their lifetime. The ISC clinic specializes in the prevention and treatment of skin cancer in patients who are immunosuppressed due to certain diseases or immune-suppressing medications.
The ISC Clinic provides information on sun protection and avoidance to help patients decrease their risk of skin cancer, and provide topical or oral treatments when appropriate to slow down or reverse sun damage. With proactive treatments and monitoring offered at the ISC, even patients who have had multiple cancers can be effectively treated and have a marked decrease in the number of new cancers they develop.
Read our Insight blog for information and inspiration about skin cancer treatment at Dana-Farber.