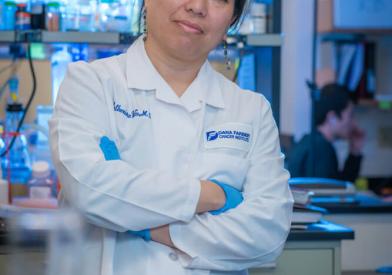
Improving Outcomes Through Innovative Science
For many patients with advanced/aggressive hematologic malignancies, allogeneic hematopoietic stem cell/bone marrow transplant (HSCT) offers the only opportunity for cure. However, some patients relapse, and many experience other complications their transplant. Our research efforts are focused on making stem cell/bone marrow transplant safer and more effective, reducing transplant-related complications, and improving immune system recovery.
As one of the largest stem cell/bone marrow transplant centers in the world, we have the clinical volume and expertise to evaluate multiple approaches to improve transplant outcomes. Our robust research enterprise is focused on several key areas:
- New treatments to better prevent or treat graft-versus-host disease (GvHD), a common and potentially severe side effect of allogeneic HSCT in which donor immune cells attack healthy patient cells and tissues
- Novel immunotherapy and vaccine therapy strategies to stimulate the curative graft-versus-tumor (GvT) effect to control disease relapse
- Therapies to address complications that arise due to the weakened immune system of stem cell transplant patients
While advances have been made, there is more work to be done. Our program currently offers more than 15 clinical trials for stem cell/bone marrow transplant patients, many of which are available only at Dana-Farber Brigham Cancer Center. Key areas of research are featured below. See a full list of our stem cell/bone marrow transplant clinical trials.
Graft-vs-Host Disease
Dana-Farber is one of the world's leading research and treatment centers for acute and chronic GvHD, a challenging complication of allogeneic HSCT that can impact both quality of life and survival. Our scientists made the groundbreaking discovery of the role that both B cells and interleukin-2 (IL-2) can have in managing GvHD, and several studies examining these approaches and other novel therapies are ongoing. Some of these trials in GvHD management and prevention are highlighted below.
Acute GVHD (aGvHD)
For patients who receive stem cells from unrelated, mismatched donors, there is an increased risk of aGvHD and infections. Despite the use of drugs such as methotrexate, tacrolimus, and cyclosporine A, many patients still suffer from acute or chronic GvHD.
- 22-190: This phase 3 study evaluates itolizumab in combination with corticosteroids for the initial treatment of acute graft-versus-host disease.
- 20-227: This phase 2 study compares a short-term dosing schedule of abatacept to an extended dosing schedule for graft-versus-host disease prevention.
Chronic GvHD
Chronic GvHD (cGvHD) remains a major complication of allogeneic HSCT, occurring in approximately 50 percent of transplant survivors and involving inflammation in multiple organs. Patients with cGvHD require prolonged immunosuppressive treatment, but some experience significant side effects and unsatisfactory outcomes, particularly patients with high-risk features of cGvHD.
- 18-499 – KD025 for Chronic Graft-versus-Host Disease
This phase 2 study evaluates KD025 for patients with chronic graft-versus-host disease (cGVHD). KD025 (also known as belumosudil) is an orally available Rho-associated coiled-coil kinase 2 (ROCK2) selective inhibitor. KD025 has been shown to downregulate pro-inflammatory T helper 17 cells and T follicular helper cells while upregulating anti-inflammatory regulatory T cells, which may potentially correct the immunological imbalance seen in cGVHD. - 16-256 – Preventing Chronic GVHD with Obinutuzumab
This randomized phase 2 trial evaluates obinutuzumab, a potent anti-B cell agent, as a preventative therapy for cGvHD after HSCT. Patients will be randomized to receive obinutuzumab or a placebo at 3, 6, 9 and 12 months after HSCT.
Relapse Therapy and Prevention
Although allogeneic HSCT is a potential curative therapy for patients with advanced hematologic cancers, disease relapse is the most frequent cause of treatment failure. Our team is pursuing novel strategies in immunotherapy and vaccine therapy to induce or restore curative GvT activity post-transplant.
- 20-336 - Enhancing Anti-Tumor Response and Managing GVHD with T-reg Enriched Cells
This pilot/phase 1 study for patients with relapsed AML or MDS explores the use Treg-enriched cells in haploidentical stem cell transplantation without post-transplant immune suppression to enhance graft-vs-leukemia effect while maintaining graft-versus-host disease control. - 18-283 – Adding Venetoclax to Transplant Conditioning
This clinical trial aims to improve the ability of standard reduced-intensity conditioning (RIC) treatment (e.g. fludarabine plus busulfan chemotherapy) to further deplete cancer cells by adding a targeted agent, venetoclax, to the regimen. In lab studies, venetoclax has increased the anti-tumor effects of the RIC therapy. In this study, our goal is to use venetoclax to help eliminate remaining or residual cancer and reduce the risk of relapse in high-risk MDS or AML patients. - 19-142 – Treg Depleted DLI Plus Ipilimumab
This study takes a novel approach to manipulating donor lymphocyte infusion (DLI) – a common therapy used to treat AML and MDS relapse after HSCT – by depleting the DLI product of immune suppressive Treg cells and combining it with an immunotherapy medication (ipilimumab), each of which has been shown to be effective in treating patients who relapse after transplant. We hypothesize that the combination therapy will be safe and will enhance our ability to cure patients with myeloid disease relapse after HSCT. - 19-265 – CIML NK Cell Therapy with IL-2
This innovative study uses cytokine-induced memory-like (CIML) NK cells in combination with IL-2 to activate an anti-leukemic response in patients with AML, MDS, or MPN who have relapsed after haploidentical HSCT. Earlier studies have shown NK cells to be effective in fighting myeloid diseases, but only for short durations. Our goal is to use CIML NK cells and IL2 to help sustain the NK cell activity against the AML, MDS, or MPN.
Infectious Disease and Supportive Care
An estimated 75 percent of patients who undergo stem cell transplantation each year develop an infectious complication. Our team has many active studies to prevent and address such complications.