What Is Liver Cancer?
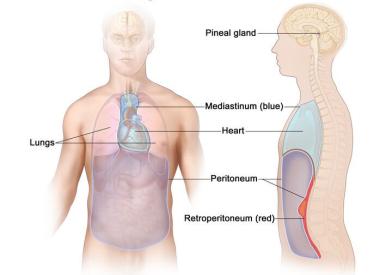
Primary liver cancer is cancer that forms in the tissues of the liver. Secondary liver cancer is cancer that spreads to the liver from another part of the body. Most liver cancer is secondary or metastatic.
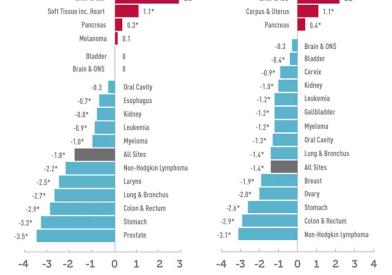
Primary liver cancer, which starts in the liver, accounts for about 2% of cancers in the U.S., but up to half of all cancers in some developing countries. This is largely due to the prevalence of hepatitis, which predisposes a person to liver cancer. In the U.S., primary liver cancer strikes twice as many men as women, at the average age of 67.
There are two types of primary liver cancer, hepatocellular carcinoma (HCC), which is most common, and intrahepatic cholangiocarcinoma (ICC).
The Liver Cancer Center at Dana-Farber Brigham Cancer Center is dedicated to treating primary liver cancer and conducting crucial research and clinical trials to learn more about the disease and develop promising new treatments.
Patients with liver cancer often require a combination of treatments. At Dana-Farber Brigham Cancer Center, all patients receive a personalized treatment plan crafted by a multidisciplinary team which includes experts in oncology, interventional radiology, surgery, radiation oncology, and hepatology. Through collaboration, our specialists are able to create a comprehensive and individualized approach to care.
Why Choose Us
At the Liver Cancer Center at Dana-Farber Brigham Cancer Center, our team of experts work together to provide compassionate and highly coordinated care for patients with primary and secondary (or metastatic) liver cancer. Our center includes leaders in the field who provide our patients with the highest level of care in state-of-the-art facilities. We also perform leading-edge basic scientific and clinical research, with numerous opportunities for patients to participate in clinical trials.
We provide comprehensive services to patients with these cancers, including:
- Access to the highest quality clinical research and new drugs available for treatment
- Support services, including nutrition, complementary therapies, spiritual support, and financial help
- Survivorship programs for patients, plus resources for families and young adults
- Multidisciplinary care delivered by specialists from Dana-Farber Cancer Institute and Brigham and Women’s Hospital